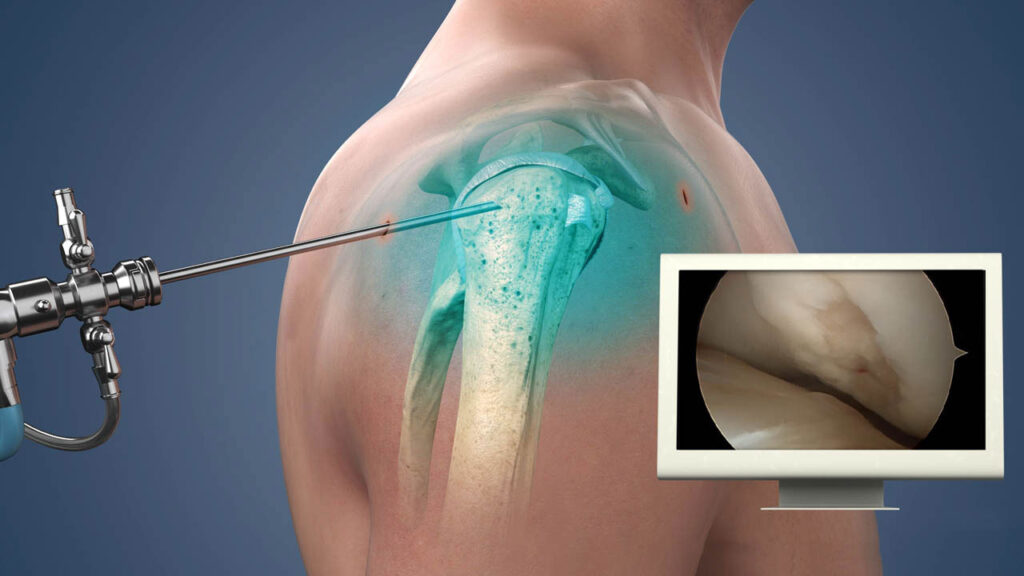
Shoulder Arthroscopy is a minimally invasive surgical procedure used to diagnose and treat various shoulder joint problems. Similar to knee arthroscopy, it involves inserting a small camera (arthroscope) into the shoulder joint through tiny incisions, allowing the surgeon to view the inside of the joint on a monitor and perform necessary procedures without needing large incisions.
Indications for Shoulder Arthroscopy:
Shoulder arthroscopy can be used to treat a wide variety of conditions affecting the shoulder joint, including:
Rotator Cuff Tears:
- The rotator cuff is a group of muscles and tendons that stabilize and move the shoulder. Tears in the rotator cuff can be partial or complete and are common in individuals who perform repetitive overhead activities, like throwing or lifting.
- Arthroscopic Treatment: Small tears may be repaired arthroscopically with sutures or anchors, while more severe tears may require tendon reattachment or reconstruction.
Shoulder Impingement Syndrome:
- This occurs when the tendons of the rotator cuff become irritated or compressed during arm movements, causing pain, especially overhead.
- Arthroscopic Treatment: The surgeon may remove bone spurs or excess tissue (such as part of the acromion bone) to create more space for the rotator cuff tendons.
Shoulder Labral Tears:
- The labrum is a cartilage structure that helps stabilize the ball-and-socket joint of the shoulder. Tears of the labrum (e.g., SLAP tears, which involve the top part of the labrum) can cause pain, instability, and a feeling of the shoulder “catching.”
- Arthroscopic Treatment: The surgeon can repair or reattach the torn labrum using sutures or anchors.
Shoulder Instability:
- Shoulder instability refers to a condition where the ball (humerus) of the shoulder joint becomes partially or completely dislocated from the socket (glenoid). This can be caused by trauma or repetitive stress.
- Arthroscopic Treatment: Arthroscopy can be used to repair damaged ligaments and tighten the joint capsule to prevent future dislocations or subluxations.
Frozen Shoulder (Adhesive Capsulitis):
- This is a condition where the shoulder becomes stiff, painful, and difficult to move due to thickening and tightening of the joint capsule.
- Arthroscopic Treatment: The surgeon may use arthroscopy to release the tight capsule or remove scar tissue, improving the range of motion.
Bicep Tendon Tears:
- The biceps tendon can tear either partially or completely, often causing pain and weakness, particularly with lifting movements.
- Arthroscopic Treatment: The torn tendon may be reattached to the bone or, in some cases, the damaged tendon may be removed if necessary.
Arthritis:
- Osteoarthritis or rheumatoid arthritis can affect the shoulder joint, causing pain, stiffness, and decreased function.
- Arthroscopic Treatment: In some cases, arthroscopy can be used to remove damaged cartilage, bone spurs, or inflamed tissue, and in some instances, the surgeon may opt for a shoulder replacement if the joint is severely damaged.
Bone Spurs or Other Bony Abnormalities:
- Bone spurs can develop on the bones of the shoulder joint, causing pain and limiting mobility.
- Arthroscopic Treatment: These spurs can be shaved or removed using arthroscopic tools.
How Shoulder Arthroscopy is Performed:
Preoperative Preparation:
- Consultation: Before the procedure, the surgeon will evaluate your shoulder’s condition through physical exams and imaging studies (e.g., X-rays or MRIs) to determine if arthroscopy is suitable.
- Anesthesia: Shoulder arthroscopy is typically performed under general anesthesia (where you are asleep), but in some cases, regional anesthesia (nerve block) may be used, numbing the shoulder and arm area.
- Positioning: The surgeon will position the patient with the arm in a way that provides easy access to the shoulder joint. The shoulder may be placed in a device called a “shoulder holder” to stabilize it during the procedure.
Surgical Procedure:
- Incisions: The surgeon will make 2 to 4 small incisions, each about 0.5–1 cm in length, around the shoulder joint. One of the incisions is used to insert the arthroscope (camera) into the joint, while other incisions are used to insert small surgical instruments for treatment.
- Inspection and Treatment: The surgeon will examine the interior of the shoulder joint on a monitor, looking for damaged structures such as the rotator cuff, labrum, or cartilage. Treatment can include:
- Debridement: Removal of damaged tissue, bone spurs, or scar tissue.
- Repair: Suturing or reattaching torn ligaments, tendons, or the labrum.
- Shaving: Removing bone spurs or abnormal cartilage to improve joint movement.
- Capsular Release: In cases of frozen shoulder, the surgeon may release tight tissue or scar tissue in the joint capsule.
- Closure: Once the necessary procedures are completed, the small incisions are closed using sutures or steri-strips. A bandage or dressing will be applied.
Postoperative Care:
- Recovery Room: After the procedure, you’ll be taken to a recovery room where you’ll be monitored as the anesthesia wears off.
- Pain Management: Pain following shoulder arthroscopy is usually mild to moderate and can be managed with oral medications and ice therapy. The surgeon may recommend a shoulder sling to support the arm for the first few days.
- Physical Therapy: Physical therapy plays an essential role in the recovery process. Therapy typically begins within the first few days after surgery and focuses on improving range of motion, strengthening muscles, and restoring function.
- Phase 1 (Initial Recovery): Focus on reducing pain and swelling, as well as gentle movement exercises.
- Phase 2 (Strengthening): Begin strengthening exercises to rebuild muscle strength and stability around the shoulder joint.
- Phase 3 (Advanced Rehab): Gradual return to normal activities, including sports or lifting, depending on the procedure and recovery progress.
- Follow-Up: You will need to attend follow-up appointments to monitor healing and ensure proper rehabilitation.
Advantages of Shoulder Arthroscopy:
- Minimally Invasive: Smaller incisions lead to less trauma to the tissues, resulting in a quicker recovery time and less postoperative pain.
- Faster Recovery: Because arthroscopy is less invasive, patients generally recover faster compared to traditional open surgery. Most people return to normal activities within 4–6 weeks, although this varies depending on the procedure.
- Reduced Risk of Infection: Smaller incisions reduce the chance of infection compared to traditional surgery.
- Better Visualization: The arthroscope provides high-definition, real-time images of the inside of the shoulder joint, enabling the surgeon to perform more accurate procedures.
- Shorter Hospital Stay: In many cases, shoulder arthroscopy is performed on an outpatient basis, meaning patients can go home the same day.
Risks and Complications:
While shoulder arthroscopy is considered a safe procedure, there are potential risks and complications, including:
- Infection: Though rare, there is a risk of infection following surgery.
- Bleeding: Some bleeding may occur during or after the procedure.
- Nerve or Blood Vessel Injury: There is a small risk of nerve or blood vessel damage during the surgery.
- Stiffness: Postoperative stiffness may occur, especially if the patient does not follow through with rehabilitation and physical therapy.
- Continued Pain: In some cases, patients may continue to experience pain or discomfort after the surgery, especially if the underlying problem wasn’t completely addressed.
- Re-injury: There’s a chance that the condition being treated may recur or that another injury may happen.
Recovery and Rehabilitation:
The recovery process after shoulder arthroscopy will vary depending on the specific procedure performed, but it typically follows these general phases:
- Immediate Post-Operative Care: You will need to rest and ice the shoulder for the first few days to reduce pain and swelling. A shoulder sling may be used for support.
- Physical Therapy: Rehabilitation typically starts early, with physical therapy exercises focused on improving range of motion and eventually strengthening the shoulder muscles. The intensity of therapy will increase gradually over several weeks.
- Return to Normal Activities: Most patients can return to light activities within 2–4 weeks, and sports or heavy lifting can be resumed within 3–6 months, depending on the nature of the procedure.


