ACL Repair (Anterior Cruciate Ligament repair) refers to the surgical procedure to fix a torn or damaged anterior cruciate ligament (ACL) in the knee. The ACL is one of the key ligaments that helps stabilize the knee joint, preventing excessive forward movement of the tibia (shin bone) relative to the femur (thigh bone) and helping to control rotation of the knee. ACL tears are common in athletes but can also occur due to accidents, falls, or other activities that put stress on the knee.
Common Causes of ACL Injury:
- Sports-Related Injuries:
- ACL tears are often associated with sports that involve cutting, pivoting, jumping, or sudden deceleration, such as basketball, soccer, football, skiing, and volleyball.
- Direct Trauma:
- A direct blow to the knee, such as in a car accident, can also cause an ACL tear.
- Improper Landing or Sudden Movements:
- Twisting or pivoting motions, especially during activities like landing from a jump or a sudden change in direction, can overstretch or tear the ACL.
- Genetic Factors:
- Some individuals may be more prone to ACL injuries due to anatomical differences in the knee joint, such as a wider pelvis or certain alignment issues that put extra stress on the ACL.
Symptoms of an ACL Tear:
The symptoms of an ACL tear can be quite distinct, especially immediately following the injury:
- A “Popping” Sound: Many people report hearing or feeling a “pop” at the time of injury.
- Severe Pain: The knee may be painful, particularly when weight is placed on it.
- Swelling: The knee can swell rapidly after the injury due to bleeding inside the joint.
- Instability: Individuals may feel that their knee is unstable or “gives way,” especially during activities that require pivoting or turning.
- Limited Range of Motion: Swelling and pain can prevent the knee from fully straightening or bending.
Diagnosis of an ACL Tear:
The diagnosis is typically made through a combination of physical examination and imaging tests:
Physical Examination:
- A doctor will perform specific tests to assess knee stability and check for signs of ACL injury, such as the Lachman test or anterior drawer test, which assess the amount of forward movement of the tibia when the knee is flexed.
Imaging:
- X-rays: Used to rule out bone fractures. X-rays do not show soft tissue like ligaments but can help identify other injuries that might be present, such as bone bruises or fractures.
- MRI (Magnetic Resonance Imaging): The most effective imaging method for visualizing soft tissue injuries like ACL tears. MRI can show the extent of the tear and any other associated injuries in the knee joint (such as damage to the meniscus, cartilage, or other ligaments).
Treatment Options for ACL Tears:
Non-Surgical Treatment (Conservative Management):
- For individuals with low activity levels, especially older adults or those who do not engage in sports or activities that put high demand on the knee, non-surgical treatment may be an option.
- Physical Therapy: A structured rehabilitation program aimed at strengthening the muscles around the knee and improving range of motion. This can help compensate for the loss of stability and prevent further injury.
- Bracing: A knee brace may provide additional support and stability.
- Activity Modification: Avoiding high-risk activities that could further damage the knee.
However, in many cases, especially for younger or more active individuals, surgery is recommended to restore full knee function and prevent further damage.
Surgical Treatment (ACL Repair/ Reconstruction):
If surgery is necessary, the procedure is typically ACL reconstruction, where the torn ligament is replaced with a graft (usually from the patient’s own body or from a donor). ACL repair, where the torn ligament is stitched back together, is much less common and typically only performed in specific circumstances.
Types of ACL Reconstruction:
Autograft (from the patient’s own body):
- Patellar Tendon Autograft: A portion of the patellar tendon is used to replace the torn ACL. This graft provides a strong and durable option but involves harvesting tissue from the kneecap area.
- Hamstring Tendon Autograft: Tendons from the hamstring muscle are used to reconstruct the ACL. This is a common method as it causes less discomfort at the donor site (the hamstring muscle).
- Quadriceps Tendon Autograft: A tendon from the quadriceps is also sometimes used, though it is less common.
Allograft (from a donor):
- In some cases, tissue from a deceased donor may be used. Allografts carry a slightly higher risk of infection or rejection but avoid harvesting tissue from the patient, allowing for a potentially quicker recovery.
Surgical Procedure:
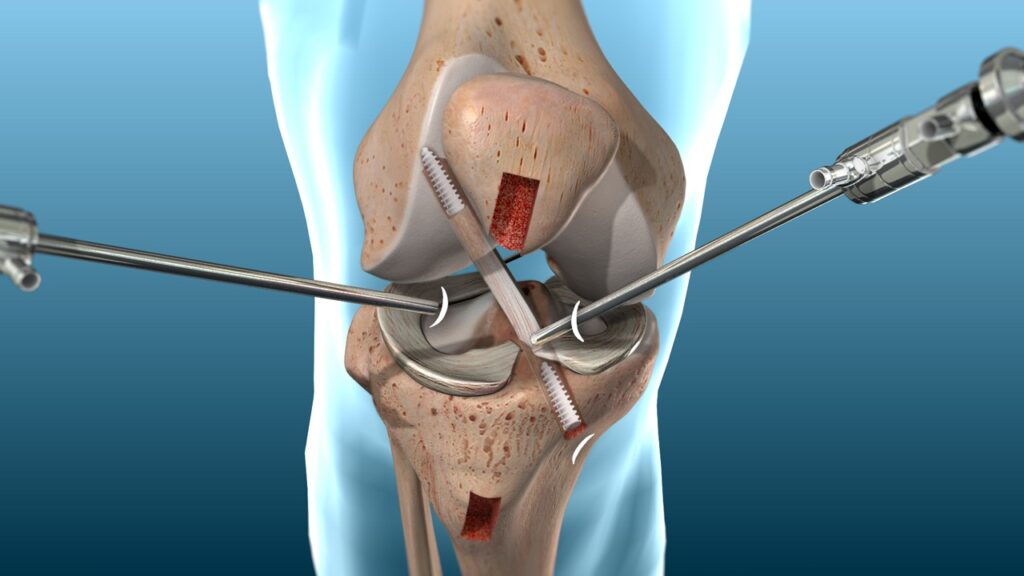
Preparation: The procedure is typically done under general anesthesia or regional anesthesia. The surgeon will make small incisions around the knee to allow for the insertion of a camera (arthroscope) and surgical instruments.
Graft Harvesting: If using an autograft, tissue will be harvested from the selected donor site (patellar tendon, hamstring tendon, or quadriceps tendon). Allografts are obtained from a donor bank.
Reconstruction: The surgeon will then prepare the area where the ACL is located, remove any remnants of the torn ligament, and drill tunnels into the femur and tibia to insert the new graft. The graft is then secured in place with screws or other fixation devices.
Post-Surgery: The procedure usually takes 1-2 hours. Afterward, the knee is typically bandaged, and a brace is often used to protect the knee during the initial recovery phase.
Recovery and Rehabilitation:
Immediate Post-Surgery:
- After surgery, the patient will usually stay in the hospital for a few hours or overnight for monitoring.
- Pain Management: Pain medications and anti-inflammatory drugs will be prescribed to manage pain and swelling. Ice and elevation are often recommended during the initial recovery phase.
Physical Therapy:
- Physical therapy begins immediately after surgery to restore knee movement, strength, and stability. Early exercises focus on regaining knee flexibility and controlling swelling.
- Strengthening: As healing progresses, the focus shifts to strengthening the quadriceps and hamstring muscles to support the knee and prevent further injury.
Weight Bearing and Mobility:
- Most patients are allowed to put weight on the knee with the help of crutches or a brace within a few days. However, weight-bearing is often limited during the first few weeks to allow the graft to heal.
- Full weight-bearing activities, including walking without crutches, usually occur within 4-6 weeks post-surgery.
Full Recovery Timeline:
- The total recovery time after ACL reconstruction is typically 6-12 months, with most patients returning to sports or high-impact activities after about 9 months to a year.
- Rehabilitation may take longer for individuals who experience complications, such as infections, graft failure, or excessive swelling.
Risks and Complications:
- Infection:
- As with any surgery, there is a risk of infection, particularly with the use of grafts.
- Graft Failure or Re-injury:
- There is a risk that the new ACL graft may fail or that the knee may be reinjured. This is why rehabilitation and proper adherence to activity restrictions are critical.
- Knee Stiffness:
- Some patients may experience difficulty in fully extending or bending the knee after surgery, which can affect long-term function.
- Blood Clots:
- As with most surgeries, there is a risk of developing blood clots, especially in the leg veins (deep vein thrombosis, or DVT).
- Nerve or Blood Vessel Injury:
- Rarely, nerves or blood vessels near the knee may be damaged during surgery.
Prognosis:
The majority of individuals who undergo ACL reconstruction experience a significant improvement in knee stability and function. Most can return to sports and normal activities, although recovery times vary. Younger athletes tend to recover more quickly, while older individuals or those with other health issues may take longer to regain full function.


